Abstract
Introduction: Venetoclax (VEN) is a highly effective agent for chronic lymphocytic leukemia (CLL) that targets BCL-2. Thus, it has been hypothesized to have efficacy in NHL and tested in phase-1/2 studies (Gerecitano JF, Blood 2015; de Vos S, Blood 2015; Davids MS, J Clin Oncol 2017). Overall response rates (ORR) observed in r/r NHL were 44% for all subtypes combined, 38% for follicular lymphoma (FL), 75% for mantle cell lymphoma (MCL), and 18% for diffuse large B-cell lymphoma (DLBCL). The adverse effect profile was consistent with the labeling despite dose escalation to doses higher than used in CLL. Additionally, VEN is a potential option in the r/r NHL setting, potentially providing less T cell toxicity compared to other agents used as bridging to T-cell therapies (Cummins NW, mBio, 2016; Dzhagalov I, J Immunol, 2008). We performed an analysis of all NHL patients (pts) treated with VEN at our institution to assess efficacy and safety of VEN in r/r NHL.
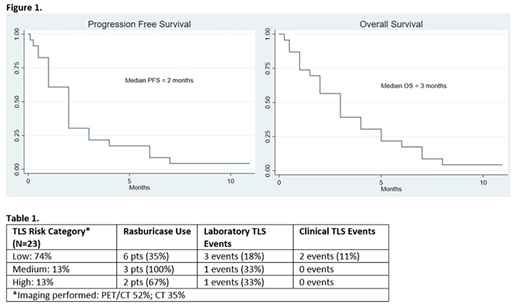
Patients and Methods: We conducted a retrospective cohort study of all adult pts who received VEN for r/r NHL at the University of Pennsylvania between 4/2016 and 6/2018. Demographics, tumor lysis syndrome (TLS; events, prophylaxis and management), duration of therapy, reason for discontinuation, overall response, survival, and toxicities were examined. The primary endpoints were progression-free survival (PFS; defined as time from VEN start to disease progression or regimen change, death due to NHL or last-follow-up in remission), and overall survival using the Kaplan-Meier method. All other analyses were descriptive.
Results: We identified 23 NHL pts for this analysis. NHL subtypes included DLBCL (35%; n=8), MCL (30%; n=7), Richter transformation (RT) (9%; n=2), transformed FL (tFL) (12%; n=4), post-transplant lymphoproliferative disease (PTLD) (4%; n=1), and marginal zone lymphoma (MZL; n=1) (4%). Median age at VEN start was 65 years; most pts were Ann Arbor stage IV (87%) and ECOG performance 2-4 (57%). NHL characteristics were MYC rearrangement (35%), BCL2 rearrangement (22%), double-hit lymphoma (26%), BCL2 IHC+ (22%), non-germinal center phenotype (13%). Median number of prior therapies was 4 (range: 2-13) with 17% having a prior autologous stem cell transplant. Median time to VEN initiation from prior therapy was 1 month (range, 0.5-9). Median VEN dose achieved was 400 mg (Range, 100-1200). Data for TLS are in Table 1. Median time on VEN was 2 months. While on VEN, 17% received radiation and 43% were on other anti-neoplastic therapy. Overall response rate (ORR) for the entire cohort was 26% (100% Partial Response [PR]). Subtypes with PR included MCL (13%), DLBCL (9%), and RT (4%). No PRs were observed with tFL, PTLD, nor MZL. Pts most commonly discontinued VEN for disease progression (74%); 2 pts (9%) remain on VEN therapy (range: 2-11 months). Median PFS and OS for the entire cohort were 2 months and 3 months, respectively, (Figure 1). Analyzed as histologic cohorts, large B-cell lymphomas (DLBCL, RT, PTLD, tFL) had similar median PFS and OS. However, small B-cell lymphomas (MCL, MZL) had median PFS and OS of 2.5 and 4 months, respectively. Two pts subsequently received CAR T-cell therapy post-VEN; one collected T-cells during VEN therapy and one collected T-cells prior to VEN start.
Adverse events (AEs) occurred in approximately 65% while on VEN. AEs included: neutropenia (48%), thrombocytopenia (43%), TLS (30%), infection (26%), neutropenic fever (26%), and diarrhea (22%). One pt had an opportunistic infection (Pneumocystis jiroveci pneumonia) while on VEN and concurrent high-dose steroids.
Conclusion: VEN monotherapy appears effective for NHL in phase I clinical trials. We describe our experience outside the setting of a clinical trial, including VEN used as part of multi-agent salvage therapy. Median PFS for our entire cohort is 2 months; AEs, while expected, were observed frequently, reflecting comorbidities. Clinical TLS events are attributed to pre-existing renal dysfunction (61% below 80 mL/min) during VEN escalation. The wide heterogeneity of VEN dose escalation, multi-agent combinations, and timing of initiation of VEN therapy are factors that require further investigation best designed as prospective clinical trials using other agents in combination with VEN.
Landsburg:Takeda: Consultancy; Curis: Consultancy, Research Funding. Schuster:Genentech: Honoraria, Research Funding; Novartis Pharmaceuticals Corporation: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Nordic Nanovector: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Merck: Consultancy, Honoraria, Research Funding; OncLive: Honoraria; Gilead: Membership on an entity's Board of Directors or advisory committees; Dava Oncology: Consultancy, Honoraria; Pfizer: Membership on an entity's Board of Directors or advisory committees; Physician's Education Source, LLC: Honoraria. Svoboda:Pharmacyclics: Consultancy, Research Funding; Bristol-Myers Squibb: Consultancy, Research Funding; TG Therapeutics: Research Funding; Seattle Genetics: Consultancy, Research Funding; Regeneron: Research Funding; KITE: Consultancy; Kyowa: Consultancy; Merck: Research Funding. Gill:Novartis: Research Funding; Extellia: Consultancy, Membership on an entity's Board of Directors or advisory committees; Carisma Therapeutics: Equity Ownership. Mato:TG Therapeutics: Consultancy, Research Funding; AstraZeneca: Consultancy; Portola: Research Funding; Johnson & Johnson: Consultancy; Regeneron: Research Funding; Acerta: Research Funding; Celgene: Consultancy; Prime Oncology: Honoraria; Pharmacyclics, an AbbVie Company: Consultancy, Research Funding; AbbVie: Consultancy, Research Funding; Medscape: Honoraria. Altman:Epizyme: Other: payment to the institution to conduct clinical trial work; Incyte: Other: payment to the institution to conduct clinical trial work; Agios: Other: Payment to the institution to conduct the trial ; Pfizer: Other: payment to the institution to conduct clinical trial work; Ariad: Other: payment to the institution to conduct clinical trial work; BMS: Membership on an entity's Board of Directors or advisory committees; Astellas Pharma: Other; GSK: Other: payment to the institution to conduct clinical trial work; Boeringer Ingelheim: Other: payment to the institution to conduct clinical trial work; FujiFilm: Other: payment to the institution to conduct clinical trial work; Celgene: Membership on an entity's Board of Directors or advisory committees, Other: payment to the institution to conduct clinical trial work; Bayer: Other: payment to the institution to conduct clinical trial work; Celator: Other: payment to the institution to conduct clinical trial work; Cyclacel: Other: payment to the institution to conduct clinical trial work; Syros: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees; Genetech: Other: Payment to the institution to conduct clinical trial work; Janssen Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees; Immune Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees. Dwivedy Nasta:Pharmacyclics: Research Funding; Incyte: Research Funding; Roche: Research Funding; Aileron: Research Funding; Rafael/WF: Research Funding; Debiopharm: Research Funding; Merck: Other: DSMC; Takeda/Millenium: Research Funding; Celgene: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal